My patient is a 78 year old female housewife hailing from a rural district in south india.
She presented to us with chief complaints of :
Patient was brought to casuality on 23/11/22 at 4:00 am early in the morning with complaints of loose stools since 5 days and pain as mentioned by the atttender as she was screaming and restless with altered sensorium.
History of presenting illness:
The patient was apparently asymptomatic 5 days ago. She passed loose stools- watery in consistency, foul smelling and blood tinged on consuming kaya churnam (an ayurvedic powder) , went to RMP nearby and was given medication, even upon which loose stools didnot stop . The attender mentions she became weak and then on 23rd nov, apparently after eating curd rice , when patient slept , suddenly in the middle of night patient was screaming due to pain and could not talk anything, as mentioned by the attender. She was then bought to casuality.
History of past illness:
The patient's attender also tells that few yrs back in 2009, she fell down in bathroom and became unconscious . She was unconscious for 10 to 15 days and during that period couldnt recognize anyone and couldnt talk and later when she was conscious, she could recognize their family members and diagnostic as hypertensive. But since then, she restricted herself to bed and didnt walk much due to fear of falling down and didnt do much work.
She is going for regular checkups once in every 3 months for BP, and weakness.
N/k/c/o Diabetes, TB or asthma., CAD, epilepsy
Addictions:
. None
Family history : His husband was a diabetic who passed away in 2008 and 1 st son is diabetic too.
Surgical history: Hysterictomised 50 yrs ago
Treatment history : Telmisartan, vit D3 , Ca2+
Personal history :
Daily routine : Patient would wake up at 6am and would have chai , biscuits , take a bath by walking with help of a walker and then have her breakfast at 8 am and would then relax , talking to her daughter in laws and would have her lunch and the attender mentioned she would have a lot of water of about 4 litres per day and sleep in the afternoon and in the evening she would talk to her grandkids and have curd rice for dinner by herself and would sleep by 10. Since 2 yrs she has not been sleeping properly and would manage only 2 - 3 hrs sleep in night. Since 5 - 6 days she is eating sabhudhana, curd rice only
Diet: mixed
Appetite : decreased
Sleep : inadequate
Bowel movements : increased since 5 days
General examination: patient was examined after taking consent from the attenders.
Pt in not cooperative and coherent qnd ia irritable.
Pallor - present
Icterus- absent
Cyanosis- absent
Clubbing- absent
Koilonychia - absent
Lymphadenopathy - absent
Edema - grade 1 pedal edema
Vitals at presentation
Bp-100/80mm Hg
PR-104 bpm
Respiratory rate : 17/min
SpO2 : 96%
Temperature : Afebrile
Systemic examination :
CVS :
No thrills, no parasternal heave,
S1, S2 +, no murmurs
Respiratory system :
.BAE +
Trachea is central in position, no dyspnoea, no wheeze, vesicular breath sounds heard
Abdomen examination :
Non tender , bowel sounds heard
CNS :
Oriented to person but not to time and place.
Repeatation : absent
Recall: absent
Language : absent
GCS : E4 V4M6
TONE : Rt Lft
U/L. Normal. Normal
L/L. Normal. Normal
Power :
U/L 3/5 3/5
L/L 3/5 3/5
Reflexes:
Right. Left.
Biceps. ++. ++
Triceps. ++. ++
Supinator ++. ++
Knee. - -
Ankle ++ ++
Plantar F F
Speech - normal
Signs of meningeal irritation - not present
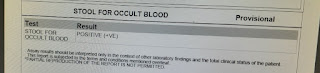
Investigations :
Provisional diagnosis :
Altered sensorium secondary to Hyponatremia (Hypovolemic Hyponatremia)(True Hyponatremia) secondary to GI loss. Dysentery with Anemia under Evaluation.
Treatment
1.INJ. NS @ 75 ml/hr
2.INJ. METRONIDAZOLE 500 MG /IV/TID
3.INJ. PAN 40 MG /IV/OD
4.IVF-ZOFER 4mg /IV/SOC
5. ORS sachet 1 in 1 litre of H20 . Drink after each episode of loose stools
6. TAB SPOROLAC - DS / FO/TID
7. Ryles tube insertion
8. INJ. Metrogyl
9. Head end elevation
10 . INJ. Monocef 1gm/IV/TID
11.Change posture 2 hourly.
12.SYP POTCHLOR 15ML in 1glass of water.









Comments
Post a Comment