DEIDENTIFICATION :
The privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever.
CONSENT :
An informed consent has been taken from the patient in the presence of the family attenders and other witnesses as well and the document has been conserved securely for future references
Documentation :
is being done on 6th of september 2022
(Updates will be done later in the future with dates mentioned for the same)
My patient is a 60 year old man , resident of ramulapeta, who is a daily wage labourer in construction work.
CHIEF COMPLAINTS
He presented to us with chief complaints of
Dry cough since 10 days
Dragging type of pain in both upper limbs since 10 days
Lower back pain since 10 days
Shortness of breath Grade 2
Chest pain near heart since 10 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 1 year ago. He then noticed involuntary movements of upper right limb at rest and decreased on movement. The patient attenders have told that he took herbal medicine but even that didnt help.
Since 20 days back he has trouble recollecting and takes at least 30-40 minutes if he wants to do something Like bringing a article from home
10 days back He had high fever which was intermittent and associated with chills lasting for 3 days.
Then 10 days back he experienced dry cough
It was relieved on medication and rest
Chest pain more of a burning sensation since 10 days
Shortness of breath Grade 2 since 10 days
Which was aggrievated on supine position and not relieved in rest.
No association with fever vomiting or headache
DAILY ROUTINE :
The patient is an mason by occupation .Usually before his ailment he used to get up in the morning by 5 am ,freshen up, have his breakfast and leave for work, lunch was usually done outdoors,evening times after returning from work he used to watch TV and,after which he usually had dinner at around 9;00pm and then go to bed.
Daily routine after pain :
Stopped going to work since 10 days, Still wakes up at 5 but then Eats and sleeps and Sometimes watches tv.
PAST HISTORY
Not a known case of Diabetes ,Hypertension, Tb, Asthma, Epilepsy, Cvd,
PERSONAL HISTORY:
After demise of his wife ( 2years ago ) he started consuming alcohol and also smoking a packet of beedi per day, but then changed since 1 year.
FAMILY HISTORY
No similar complaints in family
GENERAL PHYSICAL EXAMINATION :
I have examined the patient after obtaining informed consent and providing reassurance ,in the presence of an attendant.
Examination has been done under adequate lighting ,with appropriate exposure , in both supine and sitting posture.
Privacy of the patient has been secured.
The patient is conscious, coherent,oriented to time,space and person , cooperative .
Moderately built and nourished
Findings :
Mild Pallor
No cyanosis,clubbing,
no pedal edema
VITALS
HR: 85 beats per minute
BP:
Temperature: Afebrile
SYSTEMIC EXAMINATION :
CARDIOVASCULAR EXAMINATION :
Inspection :
Precordium :
No precordial bulges.
No engorged veins.
No scar/sinus.
No Visible pulsations :
Other findings :
Apex Beat :
Raised jvp
PALPATION :
AUSCULTATION :
S1 ,S2 heard.
RESPIRATORY SYSTEM :
AUSCULTATION:
Bilateral air entry positive
Abdominal Examination :
P/A
Hepatomegaly, slpenomegaly
CENTRAL NERVOUS SYSTEM :
Patient is conscious, coherent and cooperative, oriented to time , place.
Delay in response but able to recall
R L
TONE UL cogwheel rigidity hypertonia
Hypertonia
LL normal normal
POWER UL /5 /5
LL /5 /5
REFLEXES
R L
Biceps 2 + 2+
Triceps 2+ 2+
Supinator 2+ 2+
Knee 2+ 2+
Babinsky sign : positive
Coordination of movement
Finger nose test: normal
Gait: short shuffling gait qnd difficulty in turning around.
Tremors : resting
pill rolling movement
Sensory system :Normal
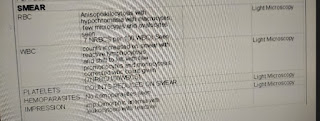
Investigations
Chest x ray taken on 4 /9/22
MRI BRAIN TAKEN ON 19 /12 /21Treatment :
Ryle's tube
Foleys catheter
IVF 3% Nacl at 10ml/hr
INJ MEROPENUM 500 mg IV/BD
INJ OPTINEURON 1 AMP IN 100 ml NS/IV/OD
INJ NEOMOL 1 gm IV/SOS
TAB DOLO
Temperature charting
Vital monitoring






























Comments
Post a Comment