CASE E-LOG
CASE SHEET
A 70 year old female came with c/o SOB since 7 days
Chief complaints:
- shortness of breath with cough
History of presenting illness:
- Patient was apparently asymptomatic 2 years back. The patient then had an episode of SOB . Now, the patient again has an episode of SOB associated with cough with expectoration , scanty sputum present .No h/o pedal edema , decreased urine output, hematuria, frothy urine.
History of past illness:
- 2 years back patient had similar complaint of shortness of breath and treated in a local hospital.
Family history :
- No relevant family history.
Personal history
- Diet : Mixed
- Appetite : decreased
- Bowel movements : Regular
- Bladder movements : Regular
General examination:
Patient is conscious, coherent and cooperative
Malnutrition+ ,mild dehydration
- Pallor: - Not seen
- Icterus: - Not seen
- Cyanosis: - Not seen
- Clubbing: - Not seen
- Koilonychia: - Not seen
- Lymphadenopathy: - Not seen
- Edema: - Not seen
- Temp: 98.7 F
- PR: 60 bpm
- BP: 110/70 mm hg
- RR: 18 cpm
- Spo2 - 98%
CVS : S1, S2 heard , No murmurs
RS :
- Position of trachea: central
- Dyspnea +
- Wheeze +
- BAE present decreased in rt side
- Expiratory wheeze + on rt IMA,ISR,IAA
- B/L Inspiratory crepts + in ISA +,IAA +
PER ABDOMEN: Soft, non tender
- Bowel sounds +
CNS:
- Patient is Conscious ,oriented to time,place and person
- HMF -intact
- Motor & sensory system: normal
- Reflexes: present
- Cranial nerves: intact
- No meningeal signs
PROVISIONAL DIAGNOSIS- ?AKI WITH COPD
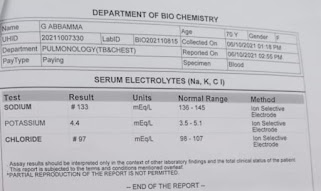
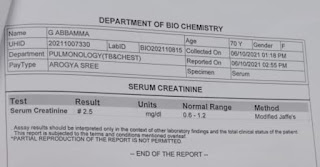
INVESTIGATIONS :
URINARY SODIUM
Day 1 soap notes :
S : SOB decreased
O : O/E
Pt is C/C/C
Temp : afebrile
BP :
PR :
CVS :S1S2 +
RS : BAE +
Tubular sounds + at rt IMA, ISA
P/A : soft , NT
CNS : : no focal deficit
A : ? PRE RENAL AkI with COPD
P :
1. IVF :NS,RL @ 50 ml / HR
2. Inj. Augmentin 2 GM IV BD
3. Inj . Pan 40 mg IV OD BBF
4. TAB. DOLO 650 MG OD SOS
5. SYP. ASCORIL.10 ML PO/ BAD
6. NEBULISATION WITH
Duolin- 8 the hourly
BuDicort -17 th hourly
Furacort - 8 th hourly
7. BP charting 8 th hourly













Comments
Post a Comment